Orthognathic Surgery
Orthognathic surgery refers to the surgical repositioning of the maxilla, mandible, and the dentoalveolar segments to achieve facial and occlusal balance. One or more segments of the jaw(s) can be simultaneously repositioned to treat various types of malocclusions and jaw deformities.

Preoperative diagnosis and planning for patients with jaw asymmetries and deformities includes a photographic analysis and a complete orthognathic work-up involving cephalometric and panorex radiographs, dental impressions, and models. This is done by the Pedodontist/Orthodontist in coordination with the craniofacial surgeon. All findings are analyzed and pre-surgical model surgery performed to ascertain the feasibility of various treatment options. Additionally, computer analysis is done pre-surgically by the craniofacial surgeon to simulate surgical results, thereby facilitating proper planning of the case. Computer analysis provides the craniofacial team with visual information and numerical data that is a compilation of many time-consuming calculations such as those used in various cephalometric analyses (Steiner, Ricketts, or Jarabak- Bjork)



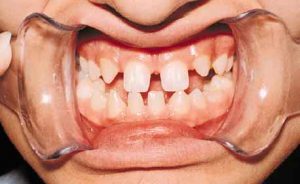
Usually, pre-surgical orthodontics are necessary to straighten the teeth and align the arches so that a stable occlusion can be obtained post-operatively, while orthodontics following surgery are frequently required to revise minor occlusal discrepancies. Orthognathic surgery is often delayed until after all of the permanent teeth have erupted unless medical conditions necessitate that the surgery be performed earlier. In adult patients, orthognathic surgery can be combined with soft tissue contouring to improve the aesthetic results.


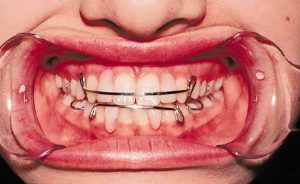
Maxillary advancement is a type of orthognathic surgery that may be necessary to improve the facial contour and normalize dental occlusion when there is a relative deficiency of the midface region. This is done by surgically moving the maxilla with sophisticated bone mobilization techniques and fixing it securely into place. For most patients, the use of screws and miniplates have replaced wiring of the bone and teeth required to hold the jaw stable. Inlay bone grafts can be utilized for space maintenance and secured with screw and plate fixation, while onlay bone grafting is used to augment the bony skeleton and improve facial soft tissue contour.


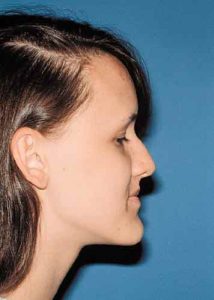
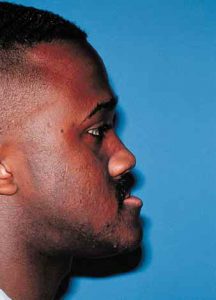
Depending on the soft tissue profile of the face or the severity of an occlusal discrepancy, problems with the lower face may require surgery on the mandible. This can be done in conjunction with or separate from maxillary surgery. The mandible can be advanced, set back, tilted or augmented with bone grafts. A combination of these procedures may be necessary. Pre-operative planning is crucial to the success of the procedure and evaluates the surgical and orthodontic options. The surgeon chooses the type of mandibular surgery based on his experience, evaluation of the photographic and cephalometric analysis, and model surgery. Following any significant surgical movement of the mandible, fixation may be accomplished with miniplates and screws or with a combination of interosseous wires and intermaxillary fixation (IMF). Rigid fixation (screws and plates) has the advantage of needing limited or no IMF. However, if interosseous wiring is used, IMF is maintained for approximately six weeks. Nutritionally balanced, blenderized diets are important for proper healing in the patient in IMF.


The chin is an important component of the facial profile as well as the aesthetic balance. The position and projection of the chin should be evaluated in patients considering orthognathic and facial soft tissue contouring procedures. Photographic and cephalometric analysis help determine the amount of change necessary to obtain a well balanced face. The chin can be augmented with such alloplastic materials as silicone, polyethylene or hydroxyapatite. However, most craniofacial surgeons prefer a sliding horizontal osteotomy genioplasty. This procedure tends to give a more natural contour to the chin and avoids the risk of extrusion that goes along with alloplastic implants.